Research in the Cardiovascular Metabolism and Inflammation Group centres on factors that influence the normal function of healthy blood vessels. A priority of the group is exploring the effects of obesity and related co-morbidities on the functioning of the cardiovascular system. There is also a cross-cutting theme of investigating the molecular basis of atherosclerosis, a disease that involves a diverse group of cells including macrophages and endothelial cells, and plays a major part in the pathogenesis of diseases such as Stroke and Type 2 Diabetes. The group uses a range of in vitro models and clinical cohorts to analyse novel biomarkers in the circulation and at both a cellular and sub-cellular level.
Nitric oxide metabolites
Nitric oxide (NO) is a gaseous free radical involved in several homeostatic mechanisms in the body. Our group is interested in the beneficial role of NO in endothelial function and in the maintenance of vascular tone.
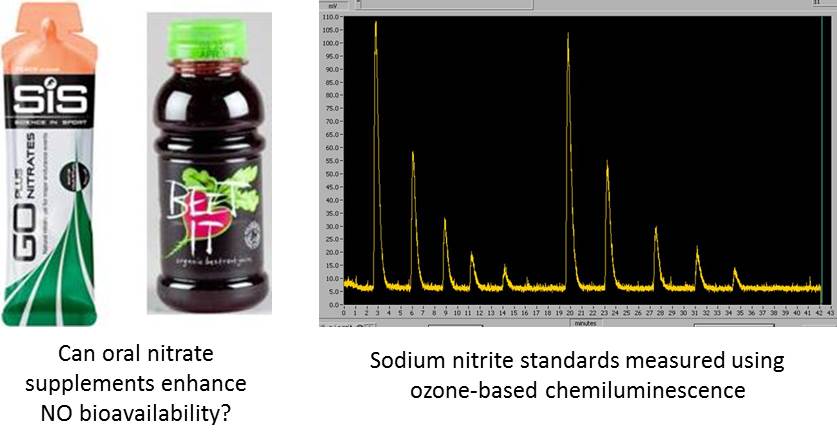
We use ozone-based chemiluminescence techniques to make high sensitivity measurements of NO metabolites such as nitrate, nitrite and nitrosothiols in blood and plasma. By profiling these metabolites in patients with different stages of cardiovascular disease, we can test whether oral nitrate supplementation enhances the circulating reservoir of NO metabolites, potentially improving the patient's cardiovascular function.
Extracellular vesicles
Extracellular vesicles (EVs) are submicron vesicles released from many cell types as intercellular communicators. EVs contain a bioactive cargo of lipids, proteins and nucleic acids that help to mediate their function and can also be used to identify EVs from complex biofluids.
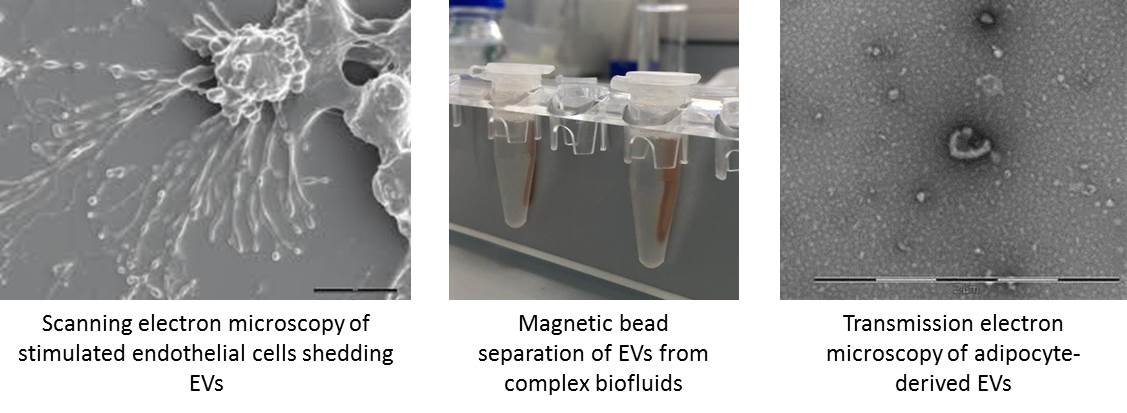
Our group is interested in the role of EVs in cardiovascular health and disease. We analyse markers carried by EVs circulating in plasma and those from primary adipocyte and endothelial cell cultures to test whether EVs can be used as disease biomarkers for cardiovascular disease and obesity. We also analyse the functional effects of these EVs on endothelial cells, leukocyte populations and isolated vessels. In addition to the biological character of EVs, we are also interested in aiding the standardisation of isolation and detection methods for EV research.
The role of inflammation in cardiovascular disease
Atherosclerosis plays a major part in the pathogenesis of diseases such as Type 2 Diabetes and its complications (cardiovascular diseases and neuroinflammatory diseases such as stroke). The pathogenesis of atherosclerosis involves a diverse group of cells including macrophages and endothelial cells. Our current interests are in how various lipids and glycosidic flavanoids can influence the inflammatory response through the regulation of macrophage polarization between the inflammatory M1 phenotype and the anti-inflammatory M2 phenotype. We are also investigating the interaction between endothelial cells and macrophages in angiogenic homeostasis. We measure these responses and interactions by monitoring the secretion of inflammatory mediators such as cytokines and the expression of regulatory transcription factors such as nuclear factor-κB (NF-κB) and the peroxisome proliferator activated receptors (PPARs), in particular PPARγ. We have recently begun to explore the modulation of EV release by saturated and unsaturated lipids and glycosidic flavanoids, and the effects of the resultant EVs on endothelial cells and macrophages.
.jpg)
The role of leukocytes in flow disturbances in the microcirculation and endothelial damage
Disturbances in the flow of blood cells and harmful interactions between blood cells and the blood vessel wall are important in the aetiology and pathophysiology of a range of diseases including cardiovascular disease and diabetes. Our research primarily focuses on how changes in the biochemistry and cytoskeletal function of cells may influence the cells biophysical properties and the flow of blood. We are able to measure the deformability of blood cells by measuring the flow through artificial models of the microcirculation using capillary-sized pores. We have also developed a model to analyse the change in leukocyte flow following alterations to the actin cytoskeleton in diseases such as diabetes. We are currently using these models to explore the role of physical activity and pharmacological intervention in normalising leukocyte biochemistry and biophysics.
.jpg)
Cardiovascular risk associated with exposure to particulate air pollution and engineered nanoparticles
Exposure to particulate air pollution and novel engineered nanoparticles presents significant risks to health. Air pollution is the world's largest environmental health risk, with
WHO estimating that 7 million people die annually as a result of exposure. The use of novel engineered nanoparticles is increasing, though their potential risks to health and the environment are unclear. Our research investigates the mechanisms by which exposure to air pollution increases cardiovascular risk, for example, by examining the effect of exposure to air pollution particles on leukocyte biochemistry and cytoskeletal function. We have recently begun experiments to monitor the interactions between leukocytes and a range of particulate pollutants, such as diesel exhaust particles and novel engineered particles including silver and iron nanoparticles.
.jpg)
Academic Associate (PhD)
Mr Mike Theodoulides,
Academic Associate (PhD)
Collaborators
Internal
Dr Jo Welton, Lecturer in Biomedical Sciences, Cardiff School of Health Sciences
Dr Shelly-Ann Evans, Senior Lecturer, Cardiff School of Health Sciences
External
Dr Aled Rees, Division of Psychological Medicine and Clinical Neurosciences, School of Medicine, Cardiff University
Dr Aled Clayton, Division of Cancer and Genetics, School of Medicine, Cardiff University
Dr Richard Anderson, Department of Cardiology, University Hospital of Wales
Dr Dev Datta, Lipid Unit, University Hospital Llandough
Professor Adrian Evans, Swansea University Medical School
Dr Kelly Bérubé, School of Biosciences, Cardiff University
Dr Timothy Higgins, School of Biosciences, Cardiff University
Professor Shareen Doak, Swansea University Medical School
Dr Martin Clift, Swansea University Medical School
Funding
Royal College of Physicians Clinical Research Fellowship to Dr Justyna Witczak, £120,417 (2015-2017). "Cell-derived microparticles as mediators of obesity-induced vascular disease" Principal Investigator: Dr Aled Rees. Co-Investigators: Professor Philip James, Dr Justyna Witczak.
British Heart Foundation Project Grant, £226,891 (2015-2018). "Extracellular vesicle transport in the circulation - a missing link between adipocytes and accelerated vascular dysfunction" Principal Investigator: Professor Philip James. Co-Investigators: Dr Aled Rees, Professor Marian Ludgate, Dr Aled Clayton, Dr Tim Hughes, Professor Valerie O'Donnell.
Cardiff University College of Biomedical & Life Sciences PhD Studentship, £75,000 (2014-2017). "Measurement of pathologically relevant microvesicle populations in obesity-driven cardiovascular disease" Principal Investigator: Professor Philip James. Co-Investigator: Dr Aled Rees.
National Institute for Social Care and Health Research PhD Studentship, £66,926 (2014-2017). "Can we prevent generation of pro-thrombotic and pro-coagulant extracellular vesicle populations in blood via a simple dietary intervention?" Principal Investigator: Dr Aled Rees. Co-Investigator: Professor Philip James.
Life Sciences National Research Network (Wales), Swansea University, Cardiff Metropolitan University PhD Studentship, £75,974 (2015-2018). "Mechanistic evaluation of the impact of superparamagnetic iron oxide nanoparticles conjugated with drugs (SPIONd) on intracellular signalling/homeostatic mechanisms. Principal Investigator: Professor Shareen Doak. Co-Investigators: Dr Rachel Adams, Dr Richard Webb.
Key Publications
Freeman PE., Moschonas KE., Hinz C., O'Donnell VB., Kinnaird TD., James PE., Anderson RA. Changes in platelet function independent of pharmacotherapy following coronary intervention in non-ST-elevation myocardial infarction patients. Atherosclerosis. 2015 Nov; 243 (1): 320-7.
Connolly KD., Guschina IA., Yeung V., Clayton A., Draman MS., Von Ruhland C., Ludgate M.,
James PE., Rees DA. Characterisation of adipocyte-derived extracellular vesicles pre- and post-adipogenesis.
Journal of Extracellular Vesicles. 2015 Nov; 4: 29159.
Higgins TP., Baker MD., Evans SA.,
Adams RA., Cobbold C. Heterogeneous responses of personalised high intensity interval training on type 2 diabetes mellitus and cardiovascular disease risk in young healthy adults.
Clinical Hemorheology and Microcirculation. 2015; 59 (4): 365-77.
Adams RA., Al-Mosawi A., Bérubé K., Jones T., Higgins T., Evans SA. Increased monocyte actin polymerization in rat blood after intratracheal instillation of air pollution particles.
Biorheology. 2014; 51 (4-5): 329-38.
